How To Manage Your Bunions Without Surgery
June 27, 2018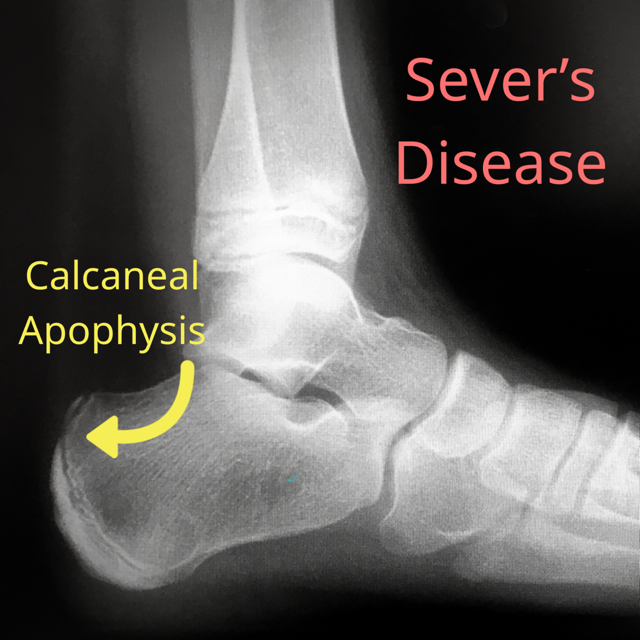
What is Sever’s Disease?
June 30, 2018Should You Have Bunion Surgery?
The #1 factor that determines if bunion surgery is necessary is the presence of PAIN. If a patient’s bunion is not painful, then I do not operate. I don’t recommend having a bunion fixed for aesthetic reasons, or to be able to squeeze into cute shoes. If a patient complains about pain to their bunion in all types of shoes, and while standing or walking, then those are justifiable reasons to move forward with bunion surgery.
Which bunion surgery is best?
There are A LOT of bunion procedures out there, and there are indications for each. Every surgeon will have bunion procedures that they prefer. It all comes down to what the surgeon is most comfortable doing, and what is indicated!
Bunion surgery can be quite technical. The more experience a surgeon has with a particular procedure, the more proficient they become at it. For this reason, patients should not suggest a specific procedure to their surgeon.
There are a couple of different procedures that I routinely use to fix bunions. What I chose depends on the bunion severity.
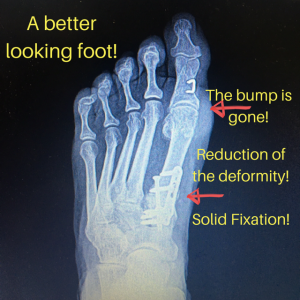
For a mild bunion deformity, I will perform a modified Austin bunionectomy. This procedure involves bone cuts at the 1st metatarsal head, then shifting the 1st metatarsal head towards the 2nd metatarsal head, and lastly fixating the 1st metatarsal with a couple screws in it’s new position. This procedure improves the 1st metatarsal phalangeal joint alignment, and gets rid of the prominent bump at the 1st metatarsal head. I plan to write a separate blog post on this procedure, so stay tuned.
For severe bunion deformities, I prefer the lapidus procedure.
What is lapidus bunion surgery?
A lapidus bunion procedure is indicated for severe bunion deformities. The procedure involves fusion of the 1st metatarsal cuneiform joint. This joint is the apex of the deformity, and hence it must be addressed.
A “severe” bunion deformity will have a very wide separation between the 1st and 2nd metatarsals. You can measure the angle between these bones on x-ray. However, if you’ve seen enough bunions, you can simply determine that the angle is well above it’s normal limits.
I also look for hypermobility at the 1st metatarsal cuneiform joint. This simply means that the ligaments surrounding the 1st metatarsal cuneiform joint have increased laxity, and the joint has a lot of up and down excursion. Fusing the joint will eliminate the hypermobility, and thus prevent recurrence of the bunion.
How is lapidus bunion surgery done?
Let me try to break down lapidus bunion surgery in the most simple terms I know (unless you are a foot surgeon, this is not a DIY tutorial):
- Make a skin excision extending from the 1st metatarsal phalangeal joint (MPJ), to the 1st metatarsal cuneiform joint (MCJ).
- Carefully dissect through soft issue until you visualize these joints.
- Free up the 1st MPJ from it’s soft tissue attachments (this will help with later reduction of the deformity).
- Remove the bump from the 1st MPJ with a saw.
- Now focus your attention to the 1st MCJ, and remove cartilage from both sides of the joint. Then prep the joint so that it bleeds well (this will allow for fusion).
- Using a saw, take a wedge off the medial cuneiform in order to close down the large angle between the 1st and 2nd
- Throw a compression screw across the 1st MCJ to make sure the joint fuses.
- Put a plate on top of the 1st MCJ, and secure the plate with screws.
- Close your incision.
How long is bunion surgery recovery time?
For a lapidus bunionectomy, I keep my patients non-weightbearing for 6 weeks. I will either put these patients in a short leg cast, or allow them to use a fracture walker (one of those big boots). The benefit of a cast is that a patient can’t remove it, so I get excellent compliance! Some patients insist on a fracture walker. I will allow these patients to wear a fracture walker for 6 weeks as long as they don’t remove it (except to shower).
Over the years, I’ve found that the patients who stay off their surgical foot for the full 6 weeks have much better outcomes that those who start walking pre-maturely.
Is bunion surgery an outpatient procedure?
Bunion surgery, regardless of the procedure, is always done in the outpatient setting.
Can a bunion come back?
A bunion can come back for a few different reasons.
- The wrong procedure was selected. For example, a lapidus bunionectomy should have been performed, but your surgeon decided to do a less aggressive metatarsal head procedure (i.e an Austin bunionectomy, which was mentioned above)
- The right procedure was selected, but inadequate correction was achieved. It is imperative to reduce the angle between the 1st and 2nd metatarsal when doing a lapidus procedure. If the angle is not sufficiently reduced, then the bunion was never truly fixed.
- The 1st MCJ did not fuse. This can occur for a number of reasons, but it usually comes down to patient non-compliance. Pre-mature weight bearing has been the most common reason that I’ve seen a failed fusion. So don’t walk on your bunion surgery until advised to do so!!!